Caremark appeals: What those Zepbound denial letters really mean
The first responses to Zepbound appeals for the CVS Caremark forced switch have started to come in. Claimable COO Alicia Graham breaks down what's in these new denial letters, and what that means next.
If you've gotten one of these letters, know that we're going to keep fighting it. We don't believe this rationale is based on medical necessity, nor that it will hold up to a secondary review. We're actively escalating these appeals, because we believe that you will win.
This thing is getting more ridiculous by the day. As we start to see responses come back to CVS Caremark, I wanted to share what we've been seeing – because frankly, a lot of what they’ve said so far is vague, misleading and even straight up false. I don't believe these denials are in compliance with the plan policy, applicable laws, or clinical standards of care at all, and we're going to break down why that Is.
This is my take on exactly what’s in these denial letters, what it actually means, and what you can do if you got one. I know how confusing this is, and I hope this can help anyone navigating it.
The one size fits all “coverage request was not approved” denial letter
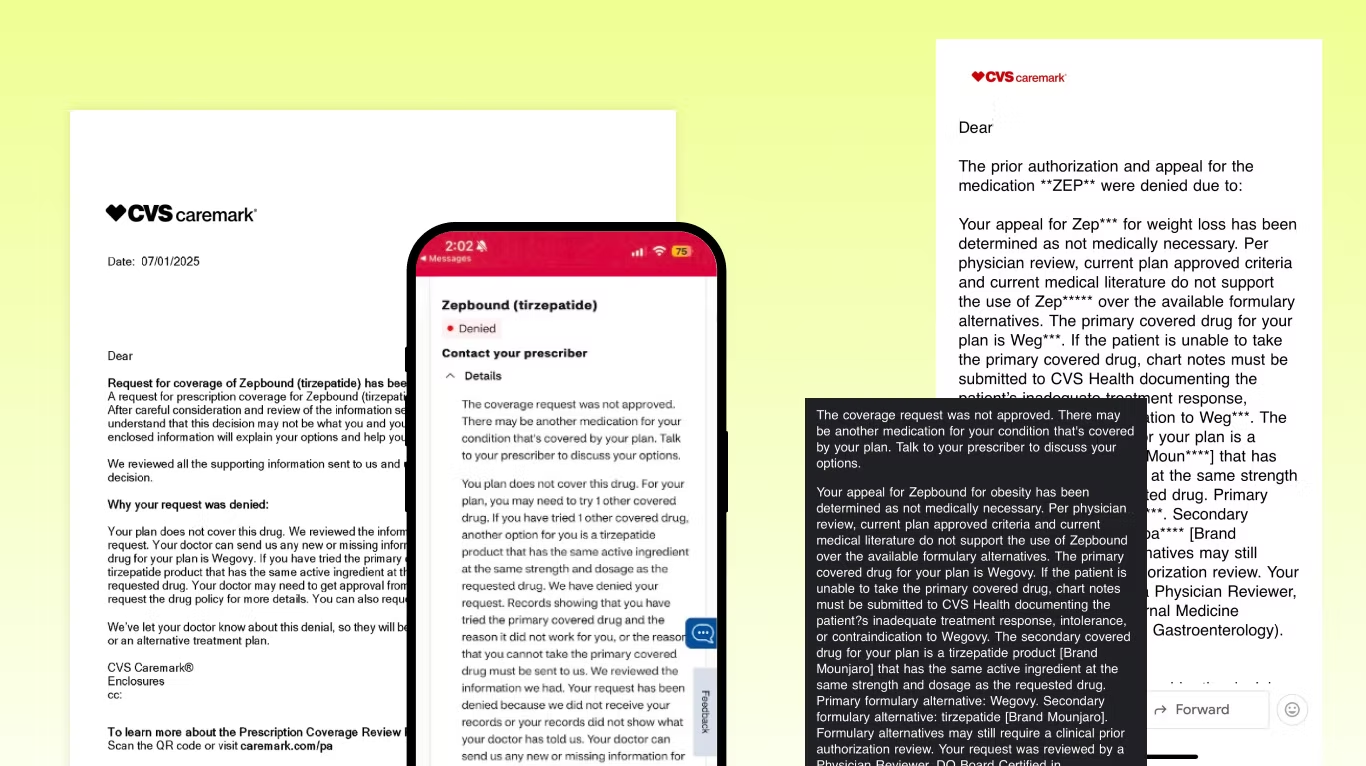
First of all, this is the language we’re seeing in almost all of these letters – just copy-pasted for everyone. By law, each appeal needs to be reviewed by a qualified human performing a full and fair review of specific case facts… so straight off the bat, it doesn’t look like they’re doing that.
“Your appeal for Zepbound has been determined as not medically necessary”
They say that current medical literature doesn’t support the use of Zepbound over the available formulary alternatives. Except it does (here's the head-to-head study we’ve been including in our appeals). They conveniently don’t include the studies they use to make their decision, which they’re supposed to do… so we have no idea why they ignored it and what they are using instead.
Plus, they’re saying Zepbound isn’t medically necessary, but Wegovy and Mounjaro are?! I don’t understand how that argument could ever stand up in a court. Wegovy is indicated for the same treatment with same coverage criteria, and Mounjaro... isn’t even indicated for weight loss.
“The primary covered drug for your plan is Wegovy”
“If the patient is unable to take the primary covered drug, chart notes must be submitted to CVS Health”. What they’re saying here is if you fail Wegovy, you could get back on Zepbound. This is step therapy, but in lots of states there are laws against this. If you live in New York, for example, they cannot require you to have previously failed Wegovy – but we’re seeing them do it anyway.
If you live in New York and got this, you should definitely fight it.
“The secondary covered drug for your plan is a tirzepatide product [Brand Mounjaro]”
This is a curveball – not what we expected to see. Yes, Mounjaro is a tirzepatide like Zepbound, but per the FDA it is only approved for type 2 diabetes.
If you and your doctor agree on you taking Mounjaro off-label, great! That’s completely up to you and what’s best for your care. But for your insurer to try to force you onto an off-label indication? Unethical, clinically absurd, and probably illegal.
But even more importantly this smells like a trap to me.
The trap: “Formulary alternatives may still require a clinical prior authorization”
They’re saying that Mounjaro may still require a PA. We’ve seen this before, so I want patients and providers to clearly understand the risk of going down this path.
The PA form states you do not qualify for Mounjaro unless you have type 2 diabetes, so the minute they ask for a PA your Mounjaro coverage will be gone. Even if they approve you without a PA today, at any time they can come back ask for it which will kick you off.
This has happened to several patients we’ve worked with who took Mounjaro for months and then were told they don’t qualify. They can force you off at any time because the criteria for Mounjaro is different.
The trap within the trap: The 180 day appeal window
I think a big part of them trying to lure you into doing Wegovy or Mounjaro is that by law, you only have 180 days to appeal your Zepbound denial. Hypothetically they could cover Mounjaro for those 180 days, and then on day 181 when that window expires and you’ve lost your right to fight for Zepbound, revoke your approval for Mounjaro – leaving you with nothing.
Even if you want to try Wegovy or Mounjaro, I would keep going on your Zepbound appeal at the same time. If you win a Zepbound appeal, they can’t just take it away.
Robocalls, app messages, and other nonsense
Legally, they have to send you a formal letter with details, full appeal rights, and more. But instead, they’re sending these mini-messages ahead of time and telling you to wait for the letter.
Why? Because not having all the info makes your response weaker and slows things down. Make sure you request your full claim file, formal denial letter, drug policy and all other decision documents. You’re legally entitled to them.
The bottom line: You don’t have to let them win
The TLDR; these denials don’t pass my smell test for compliance with the plan policy, applicable laws, or clinical standards of care. I don’t think these will hold up in external review, courts, or with regulators. So I say keep fighting.
If you got one of these, first request all the documents. Then, escalate it. In your denial letter there will be a number/address for the external reviewer to send it to. **You have the right for an external review and I think that if you do you will win.
At my company this is exactly what we’re doing. We’re creating secondary appeals that address every single piece of BS in these letters and escalating them to reviewers and regulators. Because PBMs and insurers are watching this – and the last thing I want is to show them that pulling stuff like this is ok. It’s not, and we’re going to fight it. And win.
– Alicia
PS – if you only have the “a change is coming on July 1” letter
I’ve seen a lot of people try to appeal using these letters – this will not work. This letter is not a denial of coverage for Zepbound. All this tells you that they will deny it if coverage is requested after July 1, but you can’t appeal based on this.
If you’ve only gotten this letter and want to try to stay on Zepbound, you need to get denied first. That means:
- Your provider needs to submit a new prior authorization request for Zepbound (form here)
- It’s best to do this with a LOMN attached (template here, Lilly has one also)
- You wait until that prior authorization gets denied
- Then you can appeal
Be the first to know
Get the latest updates on new tools, inspiring patient stories, expert appeal tips, and more—delivered to your inbox.
You're on the list!