Claimable Blog
Learn about appeals, denials, and stay up to date on what is happening in the world of healthcare.
Your denied healthcare claims, handled. Introducing Claimable's AI-powered platform that helps patients challenge unjust denials with custom appeal in minutes.
At Claimable, we believe everyone is entitled to the care they need and coverage they deserve. Our physician-led team of healthcare insiders, data scientists and technologists is dedicated to fighting back against the 850 million denied U.S. health claims each year, challenging baseless denials and removing barriers to care, financial strain, and medical debt.
Introducing Claimable's AI-Powered Platform
Our AI-powered platform analyzes clinical research, policy details, appeals data and your unique medical story to generate and submit customized appeals in minutes.
"This platform is a lifeline for those caught in the machinery of an industry that too often prioritizes dollars over lives."
–Wendell Potter, health insurance reform expert and former insurance executive
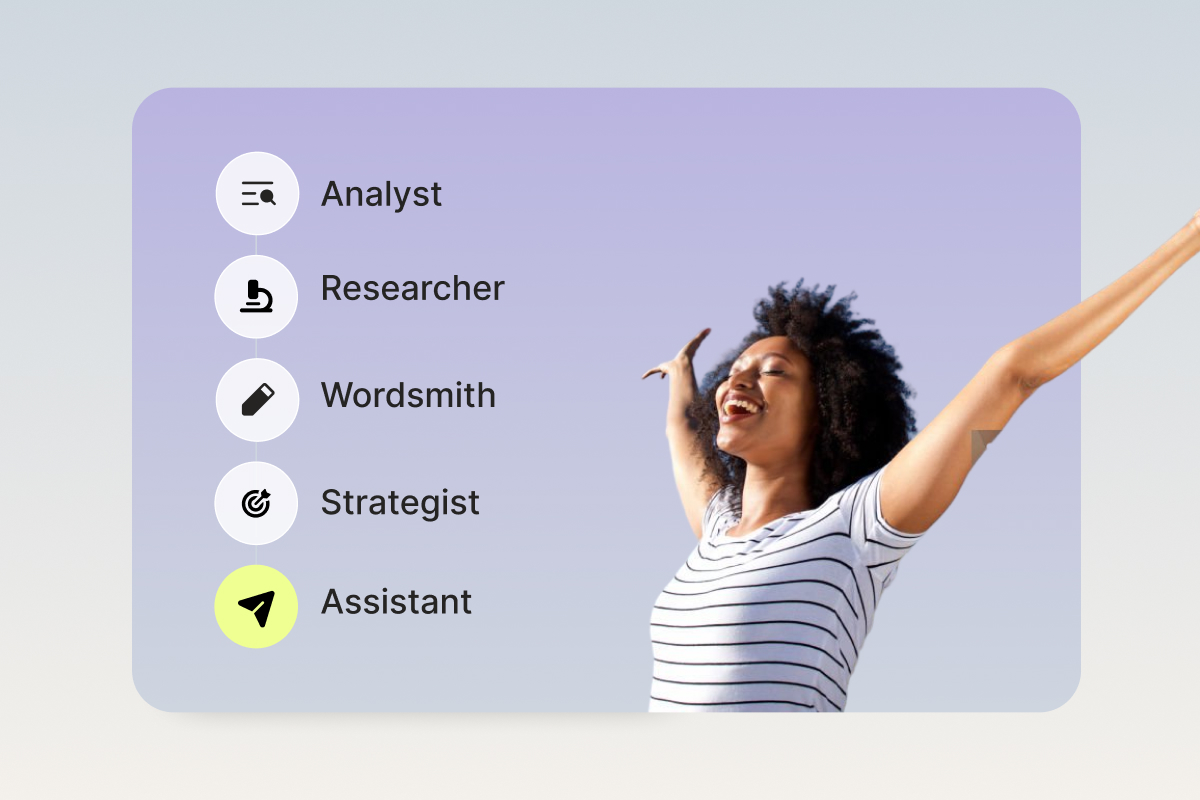
Using Claimable is like having your very own team of AI-powered experts:
Analyzer
We extract relevant details from your documents and plan policies so you don’t have to, and transform them into compelling facts and powerful stories.
Researcher
We instantly search millions of clinical guidelines, appeal precedents, policy details and legal frameworks to find evidence that supports your claim.
Strategist
We gather, review, and apply learnings from winning appeals similar to yours, ensuring you have the strongest strategy possible.
Wordsmith
We create your appeal in minutes, using our proprietary algorithm to maximize the strength of arguments, evidence, tone, voice and style.
Assistant
We help you reach the right decision-makers by taking care of letter delivery and tracking, and offer guides, reminders and tips for following up.
Breaking down your winning appeal
Claimable is your secret weapon, blending advanced technology, insider knowledge, and a library of evidence to craft customized appeals that get results.
We pull information from three important categories to craft a comprehensive, compelling appeal.
Personal Impact
Your story matters. We summarize facts, events and the personal impact of denied care on your health, life and finances.
Clinical Evidence
We illustrate the clinical justification for care, pulling from medical studies, established guidelines, claims and appeals precedents.
Policy Compliance
We include plan policies and local laws relevant to your case, demanding insurers provide specific decision details and a fair, fast appeal review.
Getting started
Our appeal builder makes the process painless, we promise. Here's what to expect:
- Eligibility check - While we are working hard to support all types of care and conditions, we currently support autoimmune and migraine related denials within the last 180 days. As a first step, we will review your denial details and let you know If Claimable can help.
- Easy document upload - You’ll start by snapping a photo of your insurance information and denial notice. This helps us save you time and ensures we don’t miss anything. No documents, no problem – you can share details manually.
- Medical history questionnaire - We'll ask you a few simple questions about the events leading up to the denial. To prepare, be ready to share what alternative treatments you’ve tried in the past and why your doctor prescribed the treatment.
- Optional extras - In some cases, sharing a statement of medical necessity from your doctor or other documentation may strengthen or expedite your case. These aren’t required, and we’ll explain how to obtain extras if you don’t have them.
You can pick up where you left off anytime and your information will be saved.
Getting a fast and fair response
Once your appeal is created, we don’t stop there. We send your appeal by Fax and First Class Mail with tracking to make sure it’s received. We request urgent, 72-hour reviews when appropriate, and typically receive standard appeal decisions within a couple weeks. In addition, we hold insurers accountable to Affordable Care Act and ERISA regulations that mandate who reviews your appeal, what they share about their decision, when they share it and how they share it.
[TABLE]
Support when you need it
We provide guidance, reminders and tips to help you take action with confidence, and offer expert support when you need it.
- Reminders and tips - Throughout the process, we offer step-by-step guidance to capture your personal story, review your draft appeal, reach the right decision-makers and follow up with insurers.
- Knowledge resources - Get answers for commonly asked questions, understand your appeal rights and process, and decode confusing terms and codes.
- Support when you need it - Our appeals team is available when you have questions, want clarifications or need extra support. We respond to support needs within 1-3 business days via email and offer live support when needed.
Getting it all at a fair, flat and affordable price
We don’t take percentage-based fees because we believe getting access to the care you need and coverage you deserve shouldn’t cost you a fortune. Instead, Claimable’s AI-powered platform delivers a powerful, efficient, affordable appeals, without having to pay thousands for a lawyer or professional advocate.
In this article, we'll help you understand the role of your doctor when appealing a denied healthcare claim, and learn how best to work together–including 7 types of information to share.
If you find yourself confused and frustrated by insurance claims and denials, you are not alone. I’m a doctor and a patient with a chronic condition. I even worked at an insurance company for a while. With all that experience under my belt, I still find the rules and processes illogical and infuriating.
The most important thing to know is that you can appeal.
It’s your right!
In this article, we’re going to talk about the role of your doctor when appealing a denial, and how best to work together––including my top 7 topics to discuss.
Do I need to involve my doctor in my appeal?
You do not need your doctor’s involvement to appeal a denied healthcare claim. There’s no set playbook and it’s unlikely your doctor is an expert (they don’t teach these things in medical school). If and how you involve your doctor is a personal choice.
It’s important to know that appealing directly can be very effective. Many doctors don’t know this is an option, and don’t advise their patients to appeal as a result. .
So what can your doctor do?
Unsurprisingly, there isn’t one simple path for your doctor to take. If your doctor's office has a lot of support staff, they may call the insurer for you and try to iron out the problem. The insurer may have your doctor speak to one of their doctors. This is something called a peer-to-peer review (though these calls can be tough to coordinate with limited peer availability for certain specialties).
Instead, your doctor might suggest you try another treatment or enroll in a Patient Assistance Program.
Discuss the trade-offs of different treatment options in terms of benefits, risks, time and costs.
7 denial topics to discuss with your doctor
The insurer might need more information to determine if the drug is appropriate or cost-effective. Below is a list of 7 items to arm your doctor with:
#1 - Symptoms
Track the frequency and severity, and share your notes with your doctor. It’s helpful to have everything formally documented in your medical records.
#2 - Impact
Explain the impact on your daily life if care is denied. For example, an inability to drive, perform your job as expected, or care for a loved one.
#3 - History
Many insurers have specific rules around what has to be tried before they will pay for certain medications. Make sure your doctor documents all other medications and treatments you’ve previously tried, and why they did not work for you.
#4 - Denial Reason
If you get a letter from the insurer, it might include a term like “denied for medical necessity,” “treatment is deemed experimental,” or “excluded benefit.” Or, perhaps you’ve concluded a trial period and need to report results to renew your medication. Knowing the reason for the denial allows your doctor to focus their conversation on the right issue.
#5 - Current Guidelines
Ask your doctor to double-check current guidelines and to document against them as much as possible. These are often the basis of the insurance company rules.
#6 - You Rights
You might need to tell your doctor that under the Affordable Care Act, your right to appeal is protected. An insurer must give you a good-faith reason as to why they denied your care.
#7 - Urgent Review
If your medical needs are urgent because you face severe harm to your physical health, you may qualify for the Insurer to review your case more rapidly - usually within 72 hours. Make sure your doctor is aware of this, if applicable.
Arming your doctor with these 7 types of information will help them advocate more effectively on your behalf.
If you’re appealing directly, your doctor can still help.
Getting a letter from your doctor stating the medical necessity and urgency of your care could help your case. This “Letter of Medical Necessity” doesn’t have to be long, but should include the condition that’s being treated, the treatment required, the reason it’s needed, and what happens if it isn’t received. It should be signed, dated, and included in your appeal.
Certain insurers may ask for seemingly random information from your doctor, such as the Tax ID number of the practice. In this case, reach out to your doctor and explain why you need this information. Your doctor wants you to get the care you need, and should gladly empower you to file an appeal.
I don’t know how to appeal. Where do I begin?
Appealing a denied healthcare claim can feel overwhelming, but don’t worry, Claimable makes it painless. Our AI-powered platform analyzes clinical research, policy details, appeals data, and your personal medical story to generate and submit customized appeals in minutes. Our Introducing, Claimable article has everything you need to know to get started. The same details you might provide to your doctor can serve as the basis for an impactful direct appeal.
Ultimately, the best advocate for your health is you.
Learn why your health insurance claim file is essential for appealing denied claims, how to request it, and what to look for when reviewing it to strengthen your case.
What is a Claim File?
A claim file contains all the documents and communications your health plan used to decide whether to approve or deny your claim. Most health plans are legally required to share this information. According to a ProPublica investigation, reviewing your claim file can help expose mistakes or misconduct by your health plan, which can make your future appeals stronger.
When Should I Request My Claim File?
You can request your claim file anytime after a denial, but we recommend doing so if your first appeal is unsuccessful. This way, you can avoid delays or extra paperwork that might interfere with a timely reconsideration. It's a smart move to have this information in hand if you need to take further steps.
Why are Claim Files Important?
Your claim file gives you insights into why your claim was denied and may reveal errors or inconsistencies that can help you in your next appeal.
Most health plans are required to provide your claim file within 30 days, so you can review it carefully.
How to Request Your Claim File
- Request Your Claim File
If you appealed through Claimable, don’t worry—we’ve already requested it as part of your appeal process. If not, you can use ProPublica's handy template to request it yourself. - Call to Follow Up
Call your insurance company’s member services team (the number’s on your insurance card) to make sure they’re processing your request. It never hurts to check in! - File a Complaint
If your insurer doesn’t provide your claim file within 30 days, it’s time to file a complaint with your state or federal regulatory agency. You’re entitled to this information.
How do I review my claim file?
Reviewing your claim file might seem daunting, but with the right checklist, you can spot important details.
Look for any missing documents or internal communications that could reveal mistakes or issues with how your claim was handled.
And remember—you can always share your claim file securely with us at Claimable if you want to participate in our ongoing research on denial issues. Just reach out at support@getclaimable.com, and we’ll send you a secure link.
Claim File Checklist
Here’s what you should look for when reviewing your file:
Does it cover the right time frame?
It should include documents leading up to, during and after your denial. If documents provided do not cover the time period stated in your claim file request–it’s incomplete.
Does it include call recordings, transcripts and call logs?
The file should contain all phone call recordings, transcripts and/or summary logs related to communications about your claims and/or denials. If you know you or your health provider called the health plan and don’t see it in the log–it’s incomplete.
Does it include email communications?
It should include emails relevant to the denial(s), including internal messages and communications with healthcare providers. If you know you or your health provider emailed the health plan and don’t see it in the file–it’s incomplete.
Does it include internal messages?
The file should include internal communications among health plan staff about the evaluation or discussion of the denial(s). If the internal reasons or evidence differ from the denial notice, you may have strong grounds to challenge the decision.
Does it include claim approval and/or denial letters?
The file should include all formal and informal notices sent to you or your healthcare provider, such as denial letters or explanation of benefits. If the denial reasons change, you may have strong grounds to challenge the decision.
Does it include prior authorization requests and responses?
The file should include documents related to requests for authorization and their subsequent approvals or denials. If it includes medical records that were subsequently re-requested or ignored, you may have strong grounds to challenge the decision.
Does it include internal memos or reports?
The file should include any written reports or memoranda related to the denial(s) that were sent by or received from health plan staff. Look for any inconsistencies between these communications and your denial.
Final Thoughts
Your claim file is a powerful tool—it can give you the information you need to fight back and strengthen your appeal. We know dealing with denials can be frustrating, but Claimable is here to help. Don't hesitate to reach out if you have questions or need guidance.

If your insurer hasn't responded to your appeal, discover how to check status and enforce review deadlines.
We know how frustrating it is to feel ignored by your insurance company, especially when your health is on the line. But you don’t have to wait endlessly—your insurer is legally required to review and respond to your appeal within set timelines.
If you haven't heard back about your appeal–here's how to hold them accountable and make sure they stick to their deadlines.
Quick Summary – More details below:
- Call member services for a status update—you deserve quick answers.
- Use the tips below to get results and avoid delay tactics.
- If you're being ignored, file a complaint with their regulator—they’re there to help!
"Never give in, never give in, never, never, never, never—in nothing, great or small, large or petty—never give in except to convictions of honor and good sense."
–Winston Churchill
How long does my insurer have to review my appeal?
The Affordable Care Act and ERISA regulations set strict rules for how appeals are handled: who reviews your appeal, how and when they must share decisions, and the specific timelines they must follow. Below are the general review timelines, but be sure to check your denial letter for specifics to your plan.
Below are the required timelines for various types of appeals.
• Expedited Service: 72 hours
• Experimental Service: 7 days
• Prior Authorization: 15 days
• Upcoming Service: 30 days
• Received Service: 60 days
You can request an expedited appeal if waiting for a claim decision may put your health at risk, such as if you urgently require medication due to a risk to health or severe pain, or are currently in the hospital. Formulary exceptions also qualify for 72 hours reviews, when you request a treatment not covered by your plan because it is medically necessary.
How do I know when my appeal was received?
We submit your appeal via Fax and First-Class Mail with tracking to ensure delivery. You’ll receive an email receipt confirming when your appeal was faxed, and mail delivery typically takes 3-5 days. If there’s an issue with delivery, we’ll let you know and work on alternative methods. If you need a detailed tracking report–reach out to support@getclaimable.com.
How can I find out my appeal status?
Call the member services number on the back of your insurance card and ask for an update on your appeal. Sometimes your provider may receive updates faster, so it’s worth checking with them too.
Can Claimable contact my insurer for me?
Your appeal is 100% yours—Claimable helps you create and send it, but we don’t contact your insurer directly or receive updates on your behalf. Because of this, you, in addition to your health provider, will be the ones to receive any updates or decisions from your insurance company.
How Can I Check My Appeal Status?
Unfortunately, insurers often use delay tactics to avoid processing appeals. Here’s how to handle common excuses:
They say: “We never received your appeal.”
You say: “I have proof it was received on [date] at [fax number] and on [date] at [address]. Please check again. I’ve also copied regulators, your CEO, and other decision-makers. Let me know if you need a detailed tracking report.”
They say: “We need more time to review.”
You say: “No, unless you can provide a valid reason in writing today that meets legal criteria for an extension. The law requires a decision within [review days], and I’ll file a complaint with [regulator] if there’s no compliance.”
They say: “You can’t appeal.”
You say: “Under the Affordable Care Act (or ERISA for self-funded plans), I have the right to appeal, including requesting exceptions to plan policies like step therapy or formularies when medically necessary. I am entitled to my own internal and external appeals, in addition to any requests or appeals sent by my health provider.”
What If I Don’t Hear Back?
Ignoring appeals is illegal. If your insurer doesn’t respond within the required timeline, you should file a complaint with your regulator—typically your state's Insurance Commissioner or the Department of Labor if you're on a self-funded plan.
Here's a breakdown of who to file a complaint with, depending on your plan type:
- Department of Labor (EBSA / ERISA): For self-funded employer plans
- State Departments of Insurance: For fully-insured employer plans, state or local government employers, and individual or exchange-purchased plans
- Centers for Medicare and Medicaid Services: For Medicare and Medicare Advantage plans
- State Medicaid Agencies: For Medicaid plans
- Office of Personnel Management : For federal employer plans

Denied your appeal? Don’t give up. Learn about your options for internal and external appeals, regulatory complaints, and legal action to fight for the care you need.
I know how frustrating it can be to receive another denial after you’ve already fought so hard. But I want to encourage you—this isn’t the end of the road. Many patients successfully win their second or even third appeal, and I’m here to help you get through this process. At Claimable, we’ve seen firsthand how persistence can pay off, and I want to make sure you have everything you need to keep moving forward.
Let’s walk through your options and how you can strengthen your next appeal.
My appeal was denied - can I file another appeal?
Yes! You have the right to multiple levels of appeal. These usually include internal reviews by your insurance company and external reviews by independent bodies. Your denial notice will explain how to re-appeal, including options for urgent cases.
How do I strengthen my next appeal?
Here’s what we’ve learned from analyzing successful appeals:
- Activate Influencers: Journalists, healthcare providers, or even industry leaders and politicians can help put pressure on insurers.
- Executive Outreach: Appeals directed to senior executives (like the CEO or medical officers) often get faster responses.
- Employer Outreach: If you’re in a self-funded plan, your employer’s leadership (like the CEO or CFO) is ultimately responsible for the plan.
- Review Your Claim File: Look for mistakes or inconsistencies that can strengthen your appeal.
- Build Your Case: If the insurer took too long, used unqualified reviewers, or broke any rules, that can boost your chances.
- Legal Support: If your case is urgent or complex, consider reaching out to a legal expert.
What are the different levels of appeal options?
STEP 1
Internal Appeals
This is your first step—ask your insurance company to reconsider. You may need to appeal twice before moving to an external review. Be sure to submit any new evidence or arguments.
STEP 2
External Appeals
An independent board will review your case and make a decision, assigning a medical expert or review board. If they overturn the denial, your insurer must comply.
STEP 3
Regulatory Complaints
If your appeals aren’t successful, you can file a complaint with a regulatory agency, which may decide to investigate and intervene on your behalf.
STEP 4
Legal Action
If all else fails, legal action may be an option. Self-funded plans, Medicare, and federal employer plans usually go to federal court, while other plans often go to state court.
Appeal Options by Health Plan Type:
Self-Funded Employer Plans (most large insurers)
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
5th: Legal Action
Relevant regulator:
Employee Benefits Security Administration (EBSA)
Fully-Insured Employer Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
5th: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
Individual / Exchange Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: Regulatory Complaint
Anytime: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
State & Local Government Employee Plans
Appeal options:
1st: Internal Review
2nd: Internal Review*
3rd: External Review
4th: Regulator Complaint
Anytime: Legal Action
Relevant regulator:
State Insurance Commissioner (NAIC)
Federal Employee Health Benefits
Appeal options:
1st: Internal Review
2nd: OPM Review
4th: MSPB Review*
5th: EEOC or OSC Complaint
Relevant regulator:
Office of Personnel Management (OPM)
Medicare & Medicare Advantage
Appeal options:
1st: Internal Review
2nd: External Review
3rd: OMHA/ALJ Hearing
4th: Appeal Council Review
5th: Judicial Review
Relevant regulator
Centers for Medicare & Medicaid Services (CMS)
Medicaid
Appeal options:
1st: Internal Review
2nd: Local Hearing*
3rd: State Hearing
4th: Office of Appeals*
5th: Legal Action
Relevant regulator:
State Medicaid Agency
* Optional or not always part of the process.
** See TRICARE and the Veterans Affairs for military or veteran related appeals.
Can Government Agencies Help?
Yes! Insurance plans are regulated by federal or state agencies that handle complaints and make sure insurers follow the rules. Here are some key regulators to know:
- Department of Labor (EBSA / ERISA): For self-funded employer plans
- State Departments of Insurance: For fully-insured employer plans, state or local government employers, and individual or exchange-purchased plans
- Centers for Medicare and Medicaid Services: For Medicare and Medicare Advantage plans
- State Medicaid Agencies: For Medicaid plans
- Office of Personnel Management : For federal employer plans
Do I Need Legal Help?
Claimable doesn’t provide legal advice, but if you’ve exhausted your appeals or face an urgent issue, legal support might help. Look for attorneys who specialize in health insurance denials—especially in cases involving bad faith or breach of contract.
Resources For Financial Help
If the costs are piling up, consider these resources:
- Patient Assistance Programs: Offered by pharmaceutical companies to provide free or discounted medications.
- Non-Profit Organizations: Groups like HealthWell Foundation, PAN Foundation or Good Days help cover treatment costs.
- Discounts, Coupons or Copay Cards: Pharmaceutical companies or third parties like GoodRx offer coupons, rebates, savings cards, free trial cards or free samples.
- Government Programs: Medicare Part D Extra Help or Medicaid offer financial aid.
- Debt Forgiveness: Programs like Undue Medical Debt or Dollar For help with medical debt relief.
Want to Learn More?
We highly recommend Marshall Allen’s book, Never Pay the First Bill: And Other Ways to Fight the Health Care System and Win, for more tips on navigating the healthcare system.
A behind the scenes look at how Claimable’s AI works to help patients level the playing field and reclaim control of their care and coverage.
What's behind our platform? Artificial intelligence is our superpower.
AI and automation have, for better or worse, become a common part of the health insurance industry. These technologies are used daily by insurers to review claims and, often unjustly, deny them.
At Claimable, we’re building AI tools that empower you - the patient. We’re leveling the playing field, leveraging technology to help you reclaim control and get the care you’re owed.
But what does that mean exactly? Let’s dive in and explore how our AI technology works, and why it gives you an appeals advantage unlike anything else.
Who are the real-life people behind your AI?
First, let me introduce myself. I’m Zach, Chief AI Officer. Before co-founding Claimable I spent nearly 15 years at the US Department of Veteran Affairs, serving most recently as Chief Data Scientist. I’m also a lecturer at the University of Iowa Tippie College of Business. All that to say, I’ve devoted my career to building innovative technologies that improve patient’s access to care.
At Claimable, my team of engineers worked hand in hand with accredited doctors and insurance insiders, spending months researching, developing, and fine-tuning our AI-powered appeals platform. And our work is never done.
As an NVIDIA Inception Program member, we continue to push the boundaries of AI innovation in healthcare. AI is evolving rapidly, as are insurance policies and regulations, and we’re constantly enhancing the experience so that you have access to the latest and greatest AI has to offer.
How is AI Being Used to Generate My Appeal?
To start, we gather the details of your case. Don’t worry, it’s easy. We’ll ask you a few questions and have you upload relevant paperwork. From there, AI takes care of the rest. Our custom-built technology takes your specific case details and cross-references them against a huge database of published medical evidence, applicable laws, and other relevant sources. Using large language models and machine learning algorithms, we synthesize large amounts of data into a clear, legally sound argument advocating for your right to receive care.
In addition to gathering relevant information, our AI is trained to recognize patterns in successful appeals and apply these insights to new cases, continually improving over time and allowing you to leverage the success of previous appeals in your own.
This is the incredible power of AI and how it gives you superhuman appeals powers, with just the click of a button.
Will It Be Personalized to My Situation, or a Form Letter?
Every appeal generated by Claimable is highly personalized. It assesses each case on its merits, considering individual patient details, medical history, and relevant precedents. Unlike generic form letters, each appeal is uniquely tailored to address the specific points of your denial, significantly improving the likelihood of a successful outcome.
Are Any Humans Involved In The Process, Or Is It 100% AI-generated?
The process of creating your appeal is done exclusively by AI. Think of it like having your very own team of AI-powered researchers, writers, and editors. The researcher and wordsmith AI draft your appeal, and the editor AI makes sure everything is correct and trustworthy. This two-step process ensures that your appeal is both correct and compelling. If there are issues with an appeal, our review team can work to resolve them.
Will It Sound Like A Robot Wrote It?
Our AI is programmed with advanced language models that produce text indistinguishable from a human professional. In other words, no robot voice here. We understand the importance of tone and language in appeals, and our AI captures them expertly. This ensures your appeal document is not only effective but also empathetic and articulate.
Will I Need to Know How to Word a Prompt?
No, you do not need to know how to word a prompt for our AI. The system is designed to be user-friendly; you simply share the necessary details of your denial, and the AI handles the rest. The Claimable experience guides you through every step of the way, no technical experience required.
I’m Not An Appeals Expert, Am I Expected To Catch Mistakes?
We don’t expect you to be an expert. Few people, including most doctors, are! That is why Claimable includes multiple layers of checks. After the initial draft is created, other AI models, trained as reviewers, analyze the content for errors or misrepresentations, correcting them before the appeal is finalized. Learn how to review an appeal here.
How Do You Prevent Hallucinations?
A hallucination is a response generated by AI that contains false or misleading information presented as fact.
To prevent hallucinations, Claimable uses only verified data sources and cross-references information across multiple databases.
If an inconsistency is detected, the system automatically flags and revises the questionable content, ensuring reliability and accuracy.
What If I Need To Reach An Actual Human For Help?
Once your appeal is ready, you'll have the opportunity to review it. If you spot anything that doesn’t look right, you can mark it for further examination. Our system is designed to catch and correct most issues automatically. However, if there’s a need for additional oversight, our team is prepared to step in and ensure everything is handled correctly, providing support when necessary.
Wouldn’t It Be Better If My Doctor Did This vs AI?
While doctors are experts in medicine, they are not trained in insurance appeals. Claimable specializes in legal argumentation and persuasive writing, often outperforming standard doctor-written appeals in terms of depth, thoroughness, and compliance with legal standards.
That said, your doctor can still support your appeal process. Learn more about how best to work with your doctor here.
How Is This Different From ChatGPT and Similar Platforms?
Unlike general-purpose AI models like ChatGPT, Claimable is specifically designed for medical legal appeals, making it far more effective and precise for your specific needs.
It not only stays updated with the latest medical evidence, legal changes and recent case developments but is also built to comply strictly with HIPAA regulations. This ensures that all your personal and medical information is handled with the utmost security and confidentiality, safeguarding your privacy throughout the process. This tailored focus and commitment to compliance make Claimable uniquely reliable and secure for handling sensitive medical appeals.
Is My Health Information Safe?
All of your data is handled with strict adherence to HIPAA regulations, ensuring your personal information is protected with the highest standards of security and confidentiality. Claimable uses encrypted data storage and transmission protocols to safeguard your information from unauthorized access.
When it comes to insurance appeals, we believe everyone is entitled to fast, affordable, effective support.
Lawyers are expensive, and doing it yourself takes huge amounts of time and expertise that most of us just don’t have. By leveraging Claimable’s AI-powered platform, you have access to a powerful, efficient, cost-effective, and safe solution, right in the palm of your hand. Insurers are making technology work for them, it’s time you do too.
Let's get you covered.
