Sucraid® insurance, approved

Claimable can help you get the coverage you need.
Evidence-backed appeals tailored to your unique situation.
How it works
Claimable partners directly with your pharmacy to make it fast and easy.

What’s in your winning appeal?
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Each month, I endure about eight major episodes, each one leaving me exhausted, unable to concentrate, and too unwell to take part in daily life.
The frequency and unpredictability of these symptoms have isolated me socially and limited my capacity to take part in activities most people take for granted.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Compelling evidence published by Hackenmueller et al. (2016) confirms that the accepted reference range for normal sucrase activity is approximately 54 μmol/min/g, with a CSID diagnosis established by a sucrase activity level of ≤25 μmol/min/g.
///////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Your denial is also contrary to established insurance precedent. Multiple independent review organizations and appeal panels have overturned denials for Sucraid in cases matching my own (see Precedent Summary).
These decisions emphasize that insurance plans must align their criteria with current scientific understanding rather than deny on arbitrary or outdated cutoffs
/////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////

Why appeal with Claimable?
From start to send in minutes
Let’s get you covered.

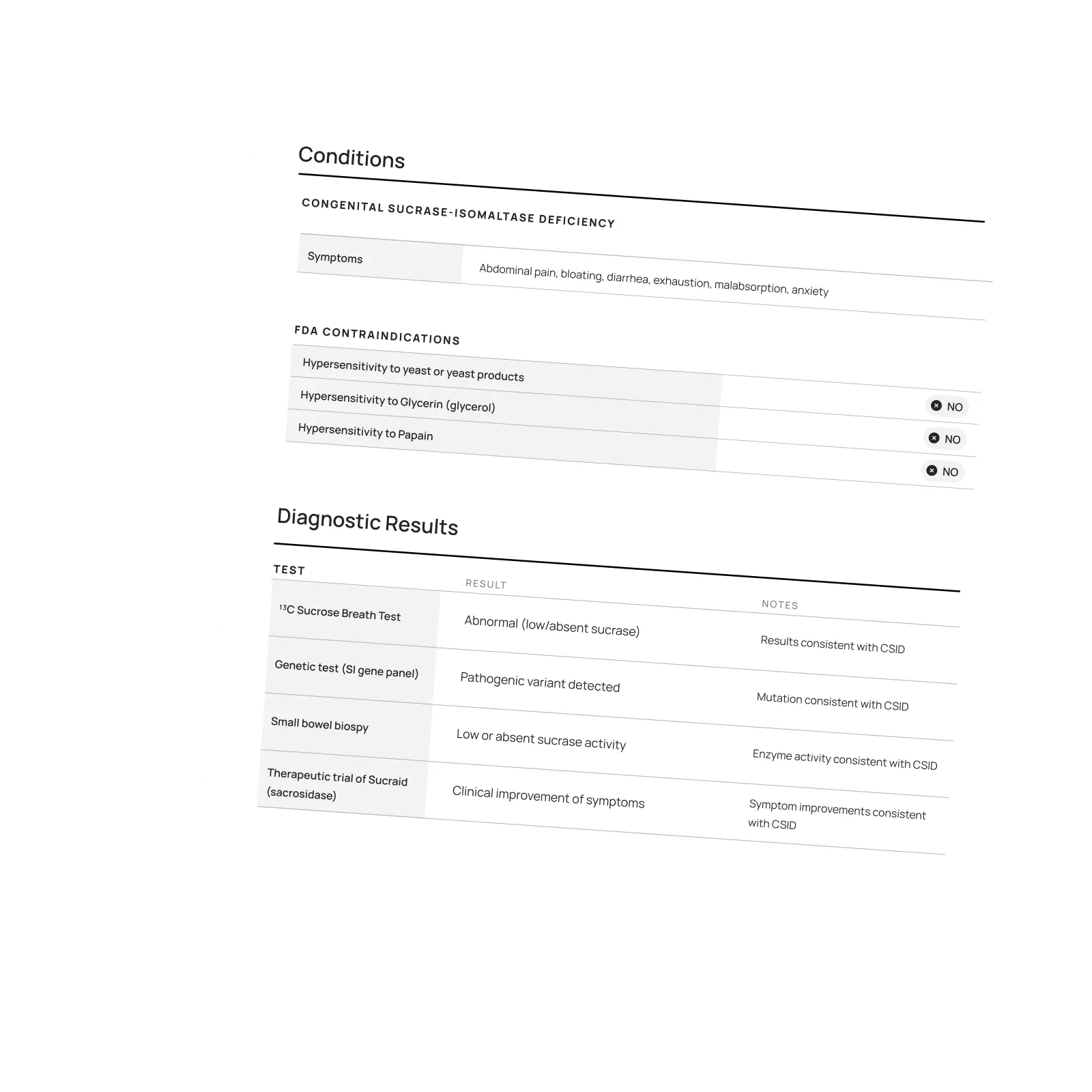
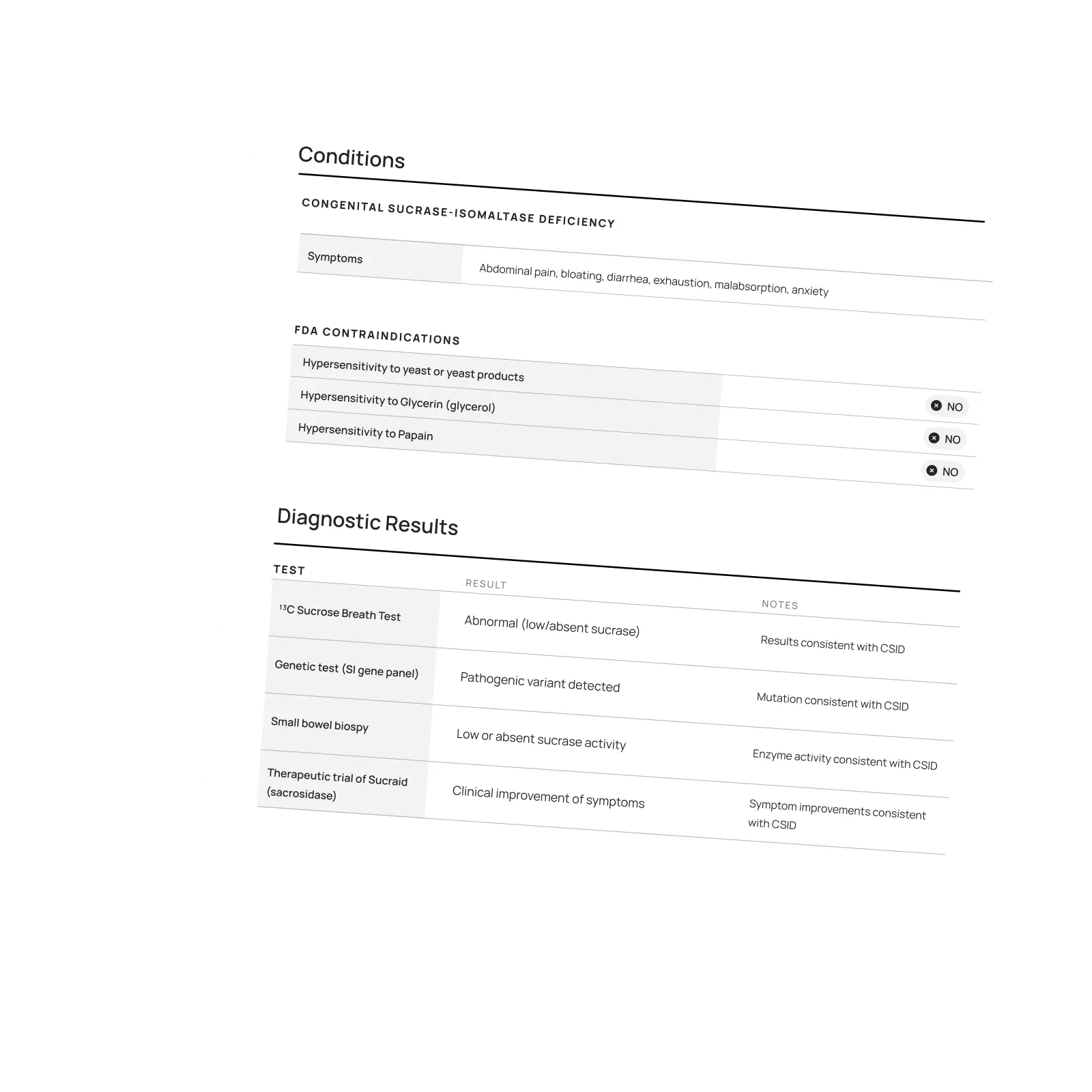
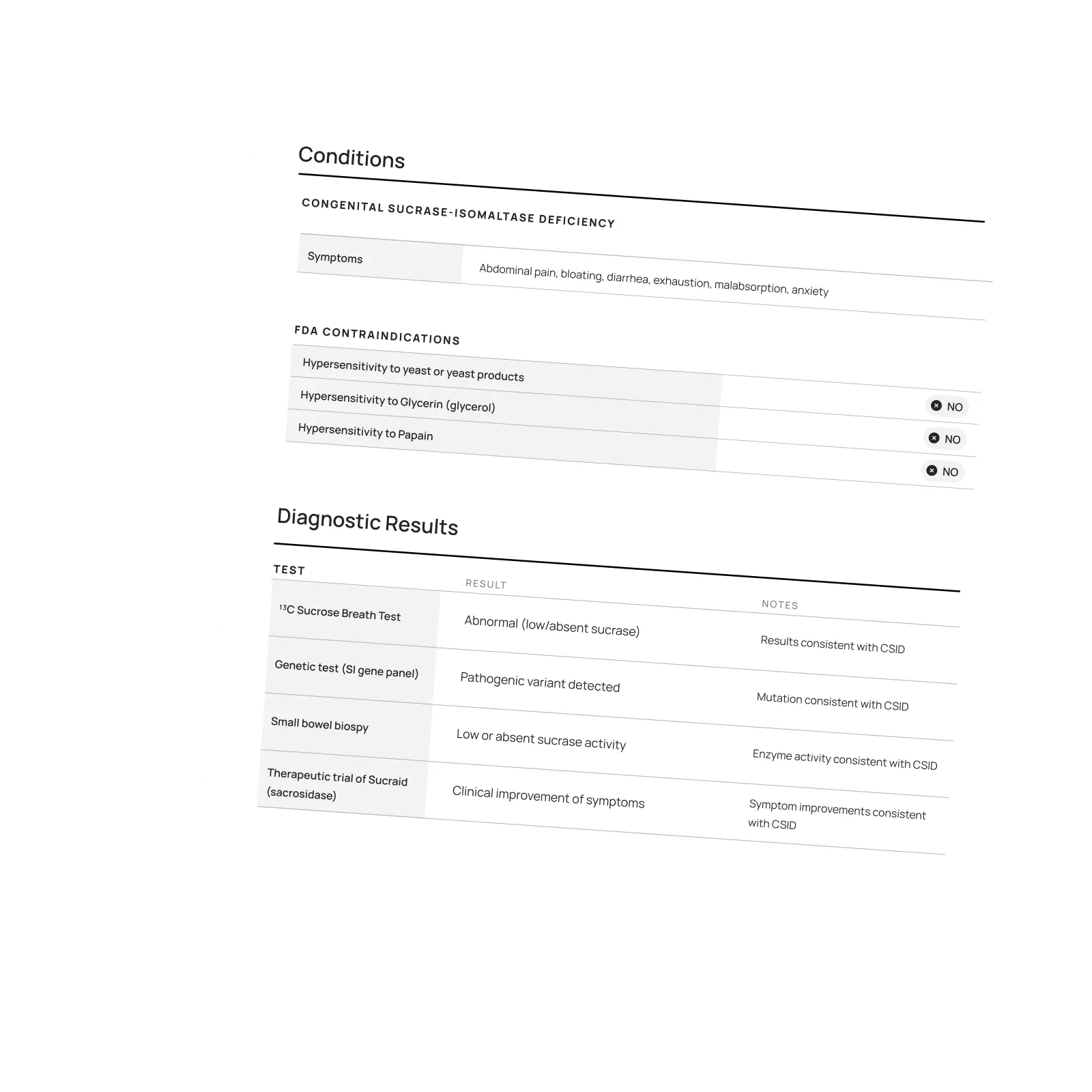
Most insurers will cover Sucraid®—but they rarely make it easy. Coverage almost always requires prior authorization based on proof of a confirmed CSID diagnosis, shown through a sucrose breath test, small bowel biopsy, or genetic test. Some plans go further, demanding invasive endoscopy or rejecting coverage when sucrase levels are “too low,” even when generally-accepted clinical standards are met. Claimable frequently helps patients challenge these unnecessary barriers—especially when insurers deny coverage or renewals that meet their own policy criteria, or when outdated plan rules fail to reflect current clinical standards.
Start by contacting your specialty pharmacy. They can coordinate a provider appeal using your doctor’s diagnostic documentation and letter of medical necessity. If that doesn’t resolve it—or if your provider can’t take on the appeal—Claimable can step in to help you file a patient appeal that builds on existing evidence and adds a complete, patient-centered narrative supported by expert policy and clinical analysis.
Federal law requires insurers to review prior authorization appeals within 15 days, though external reviews can take 30–45 days. Urgent appeals must be decided within 72 hours. Preparing and submitting your appeal with Claimable typically takes just 15–30 minutes. We track every step and help ensure your insurer meets its legal obligation to provide a timely, fair, and individualized review.
Claimable needs your consent to access your medical and insurance records so we can pick up where your pharmacy and provider left off, saving you time and effort. If you’re an adult patient, you’ll sign the form yourself. If the patient is a minor, a parent or legal guardian signs on their behalf. If the patient can’t legally consent—such as due to disability or medical incapacity—a legal guardian or authorized personal representative (like someone with medical power of attorney) must sign instead.
In some cases, such as divorced or separated parents with joint custody or co-guardians who share authority, both authorized individuals must sign before Claimable can access records. The person signing should always note their relationship to the patient. Use the Single Signer HIPAA Consent Form if only one person needs to sign, or the Co-Signer HIPAA Consent Form if two people share legal authority. For more details, see the HHS HIPAA Privacy Guidance.
Yes. The SucraidASSIST™ program, provided by QOL Medical, LLC, offers comprehensive support services for patients with CSID, their caregivers, and healthcare providers. Financial assistance may be available for patients who meet certain income and other eligibility requirements. Both the specialty pharmacy that dispenses Sucraid® and SucraidASSIST™ can provide guidance in applying for financial assistance.
Sucraid® is the only FDA-approved enzyme replacement therapy indicated for the treatment of sucrase deficiency, which is part of Congenital Sucrase-Isomaltase Deficiency (CSID), in adults and children 5 months of age and older. It provides a substitute for the sucrase enzyme in the small intestine that is missing or not working in people who have CSID.
Congenital Sucrase-Isomaltase Deficiency (CSID), also known as Genetic Sucrase-Isomaltase Deficiency (GSID), is an inherited disorder that reduces the effectiveness of enzymes that digest carbohydrates (sugars and starches). These digestive enzymes may be missing or not work properly in people with CSID.
Claimable is free for all qualifying CSID patients appealing a Sucraid® prior authorization denial. We partner directly with Sucraid® patient support programs so patients never pay out of pocket for this service. If you’re appealing another type of denial, our team can confirm whether your case qualifies for free or low-cost patient pricing.
Even the most dedicated doctors and pharmacies face limits on how much time they can spend fighting denials. When patients take the lead, the appeal reflects their full story—the impact, urgency, and details that often get lost in clinical paperwork. Claimable helps you do exactly that, combining your provider’s documentation with your personal experience to create a stronger, more persuasive appeal. 👉 Learn more: Why you should appeal your insurance denial yourself
No problem. Start by contacting your specialty pharmacy—they can resend your invite or confirm your case status. If you still can’t access your appeal, reach out directly to support@getclaimable.com and we’ll help you get started right away.








