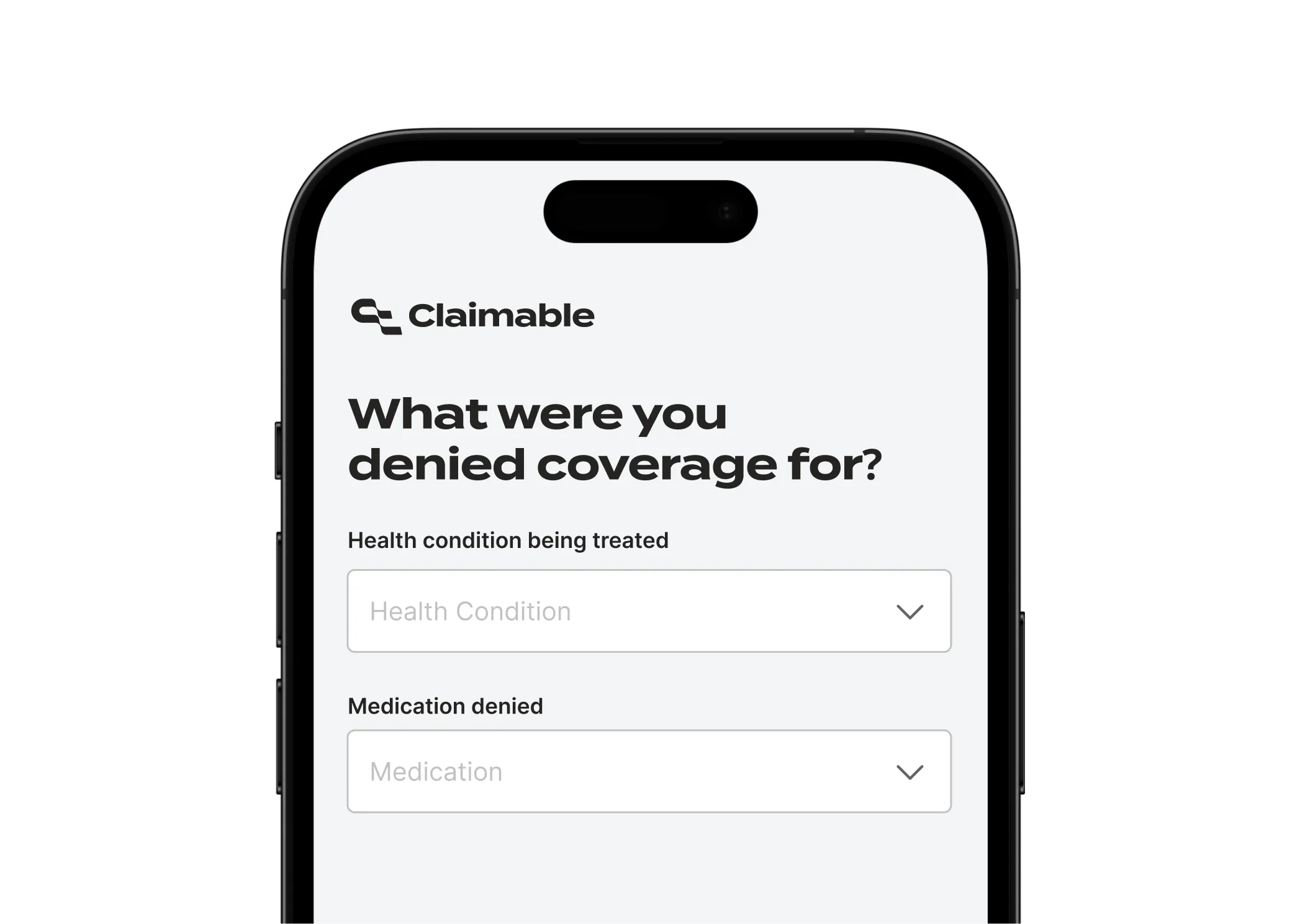
Unlock Zepbound coverage

When insurance says no, we help you get covered
Designed to fight Zepbound switches
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
I have battled obesity for much of my adult life, a struggle complicated by autoimmune and metabolic disorders. This challenge is more than just numbers on a scale; it infiltrates every aspect of my life with severe physical and emotional consequences.
I endure persistent fatigue—so overwhelming that daily activities feel akin to carrying a house on my back—paired with chronic pain in my joints and relentless back pain.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
The requirement to fail non-GLP-1 weight loss therapies before using a medication like Zepbound does not reflect the prevailing scientific consensus or best practice guidelines.
Contemporary obesity treatment guidelines—and a robust body of published research—now position GLP-1-based therapies, particularly tirzepatide, as the standard of care for patients with obesity and metabolic complications. This is substantiated by several landmark studies cited below.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
Federal law mandates comprehensive coverage of essential health benefits and prohibits unreasonable denials of medically necessary interventions. As a patient and policyholder, I am invoking my right, under this act, to a thorough review of your coverage denial, based on a fair assessment of the clinical evidence and in light of prevailing standards of care.
Continued enforcement of an outdated step therapy protocol, after documented failures with prior agents and mounting scientific consensus supporting tirzepatide, would contravene the spirit and letter of these protections.
///////////////////////////////////////////////////////////////////////
//////////////////////////////////////////////////////////////////////////
////////////////////////////////////////////////////////////////////
/////////////////////////////////////////////
How Claimable helps you win appeals




What's inside your appeal pack?

Why appeal with Claimable?
From start to send in minutes
Let's get you covered.

When insurance denies coverage for a medication, you can appeal. Appeals happen after your provider prescribes something – typically completing a prior authorization form in advance.
Once you receive a denial letter from your insurance, you can start the appeals process. To learn more about why insurers deny coverage for GLP-1s and the specific tactics we take to fight back, click here.
Creating and sending your appeal with Claimable takes just minutes.
Once you've submitted, your insurer must respond within the review period mandated by applicable laws – ranging from 72 hours for urgent to 30 days for upcoming. We request urgent reviews when appropriate – such as cases where your coverage has been dropped, and you're at risk of a care gap – and typically receive standard appeal decisions within a couple weeks.
Both options can work, but generally we recommend that you appeal with your provider's Letter of Medical Necessity attached. Patient appeals have stronger legal rights, are entitled to multiple appeals, and typically mandate responses on faster timelines.
Claimable can help you challenge initial and continuation coverage denials related to medical necessity, step therapy, forced switches, formulary exclusions, out-of-network care, site-of-care exclusions, and more. Learn more about how we help you fight back.
We currently support Zepbound and Wegovy for obesity and related co-morbidities, and Ozempic, Mounjaro, and Rybelsus for type 2 diabetes.
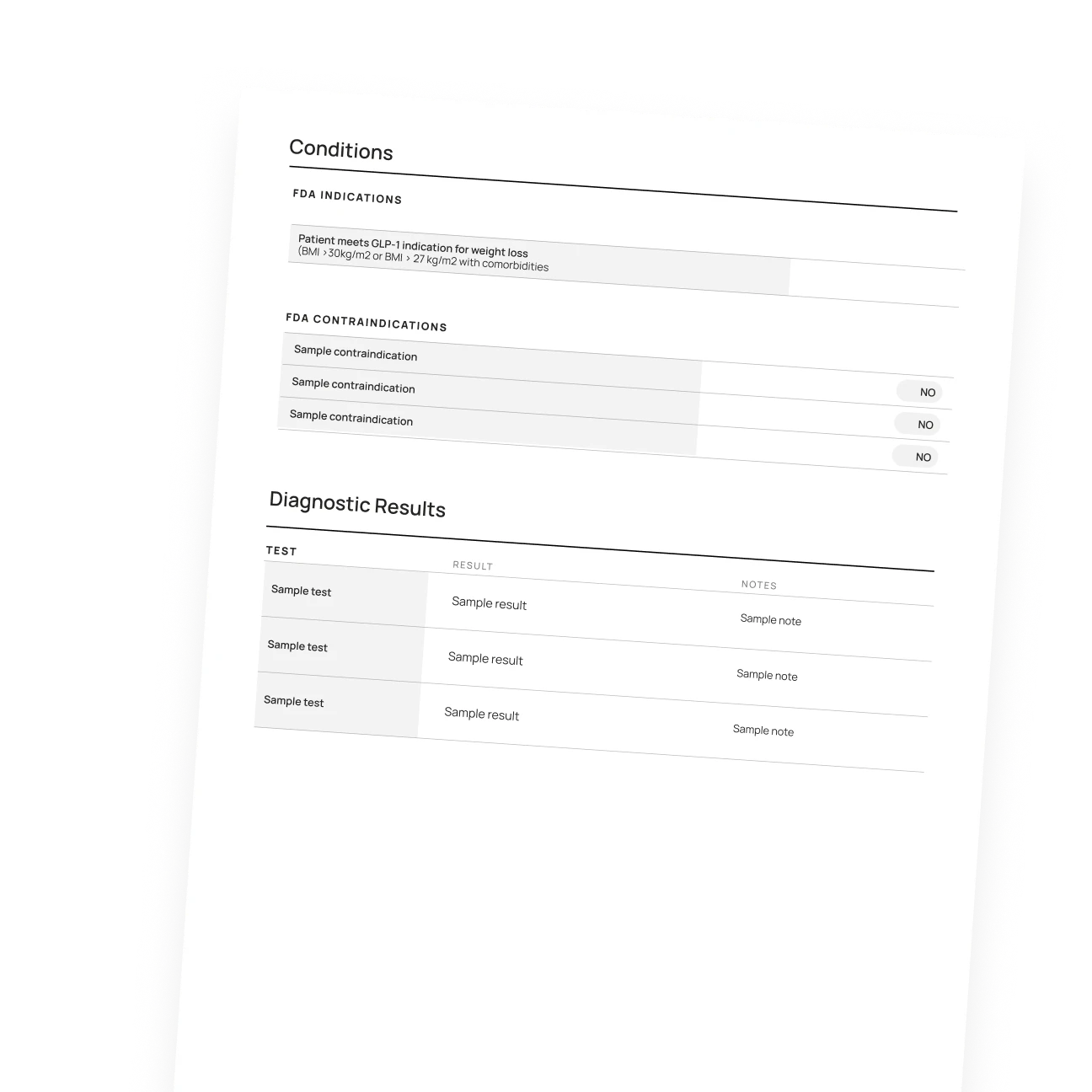
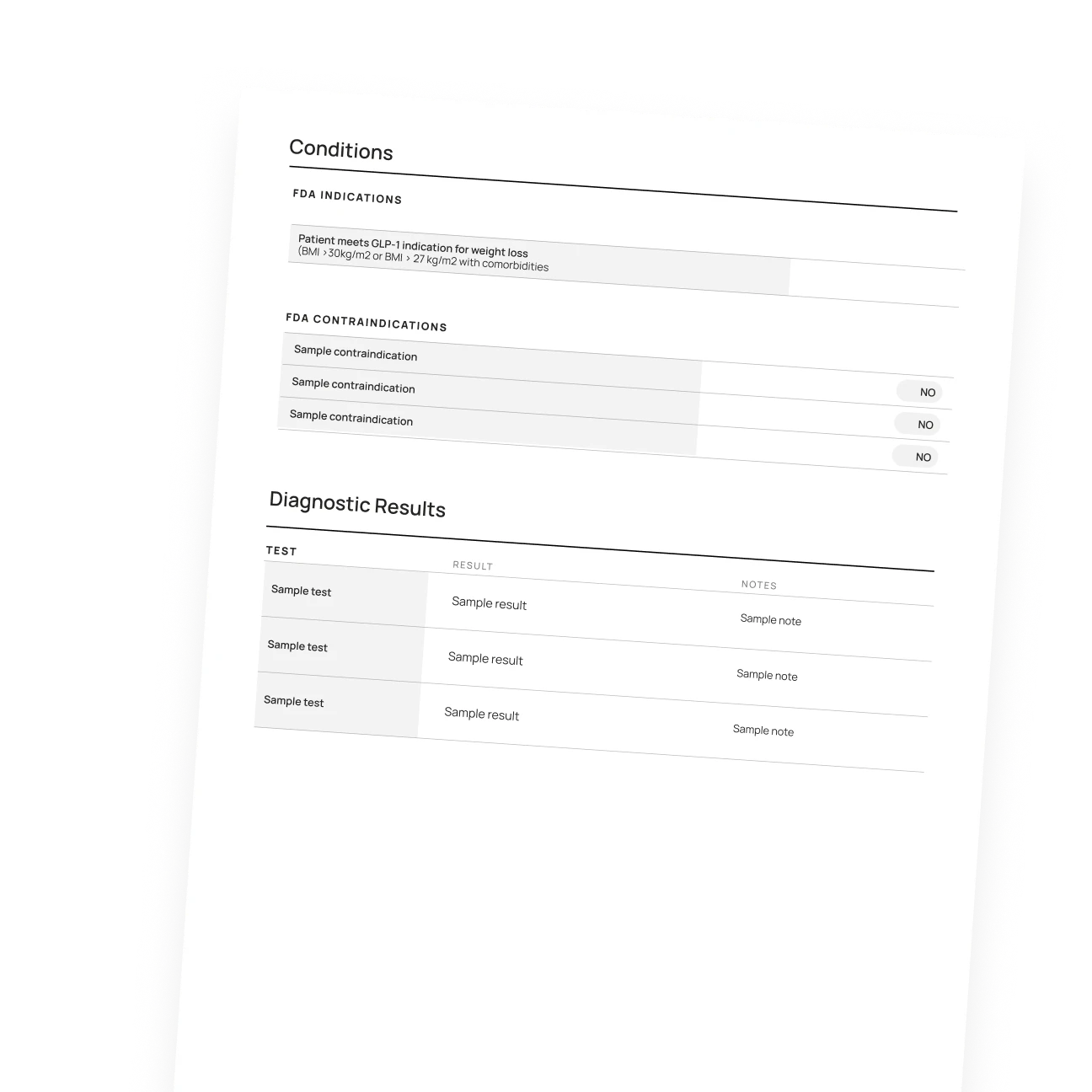
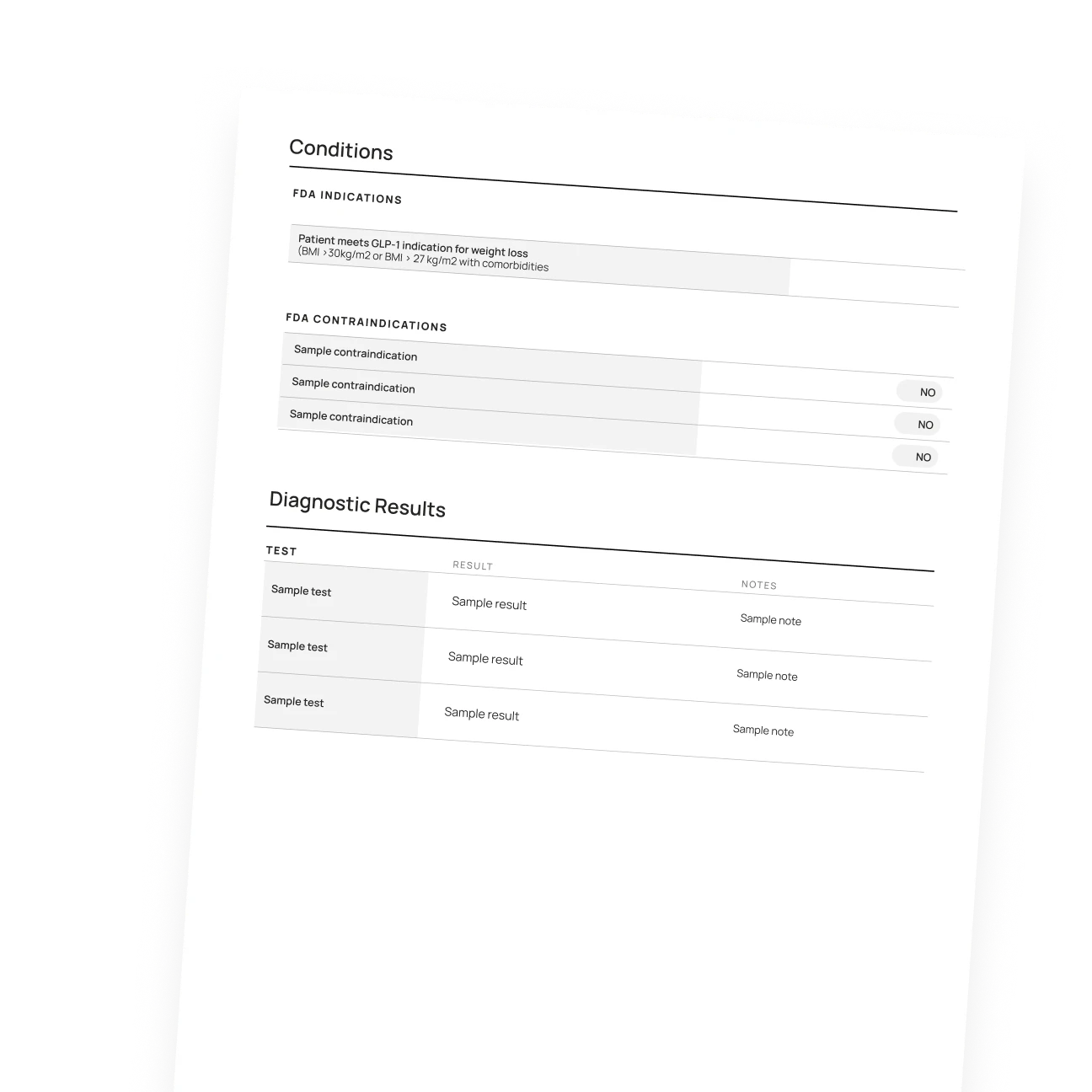
A strong appeal letter should include the following:
- Your medical results on your current medication (weight loss, symptom control, etc.)
- Any prior medications that you’ve tried and failed
- Specific medical conditions that are treated by your medication (like Zepbound for OSA)
- A letter from your doctor supporting continued use
- Clinical studies, applicable laws and insurance regulations, and precedents from successful appeals with similar cases to yours
- Supporting evidence like lab results, weight logs, dosing history and medical records
Claimable's appeals are custom built to include all of these things, personalized with your specific medical history and situation.
You have the legal right to a full, fair, and timely appeal reviewed by a qualified (human) clinician — typically within 15 days for GLP-1 denials. If your first appeal is denied, you have the right to keep appealing. Learn more about your appeal rights.









